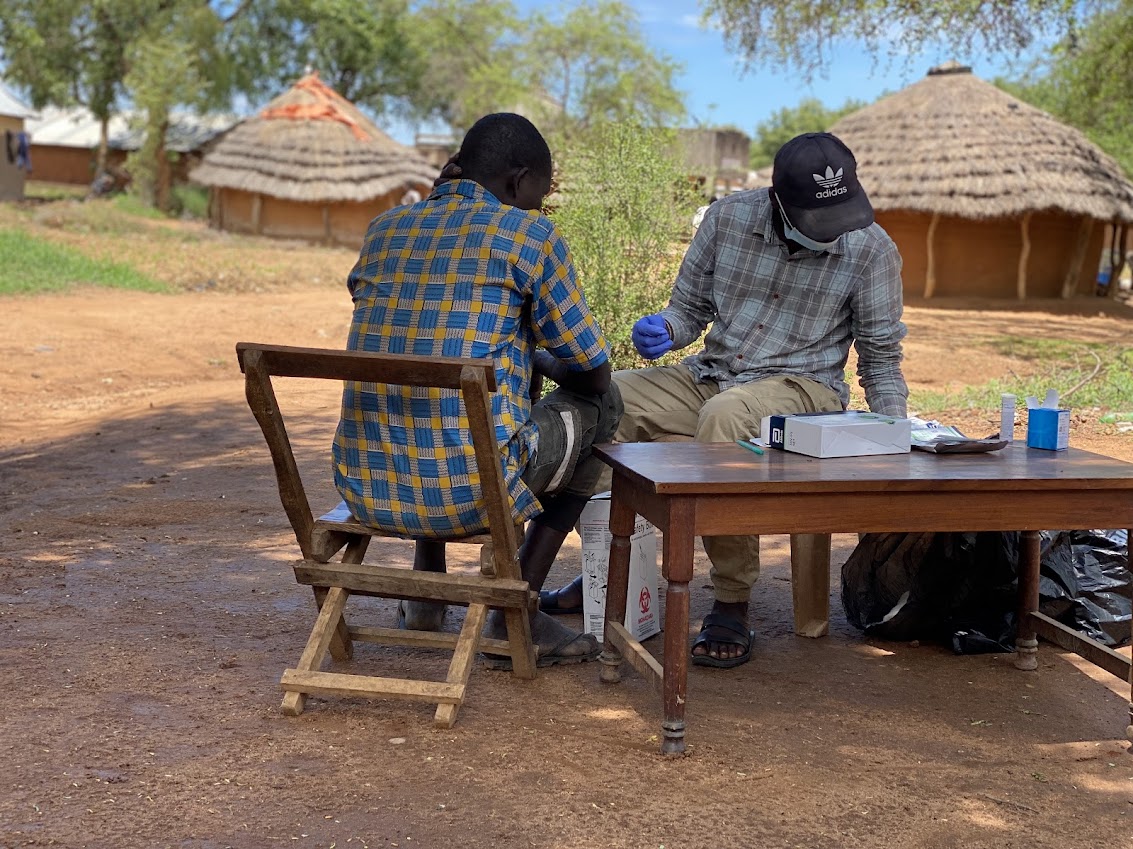
In the remote Karamoja region, Lokales Health Centre II in Amudat district is transforming healthcare by integrating HIV services into community health service delivery. This innovative approach has brought essential care to underserved communities, thanks to dedicated health workers like Madina, a counsellor with over five years of experience.
Madina tirelessly delivers integrated community health services to hard-to-reach areas, including mining sites and grazing lands. She provides HIV testing, counselling, and supports clients in achieving viral suppression, while offering other essential services such as malaria testing, Hepatitis B screening, and maternal health education. Her cultural understanding fosters trust within the community, encouraging more people to seek care.
The integrated services address the unique needs of the nomadic Karimojong lifestyle. Akiru*, a young mother, shared her experience: “I was afraid to know my status. But when Madina came to our village, she helped me understand the importance of testing. Today, I’m healthy, and my baby is HIV-free.”
Under Madina’s leadership, HIV case identification, linkage to care, and client retention have improved. Weekly outreach to high-risk hotspots like Cheptakol mining areas and Tingas trading centers ensures timely care. She also distributes HIV self-testing kits, making it easier for individuals to know their status privately.
Madina’s commitment extends to achieving viral suppression, implementing the ICSDM model, and linking non-suppressed clients to community health workers for Directly Observed Therapy (DOTs).
Despite logistical challenges, this integrated community health service delivery model has brought healthcare closer to communities, fostering ownership and responsibility for health outcomes. For Madina, the reward is clear: “When I see someone smile because they’ve regained their health, it makes everything worthwhile.” Lokales HCII demonstrates that innovation and commitment can transform even the most underserved communities.
Results:
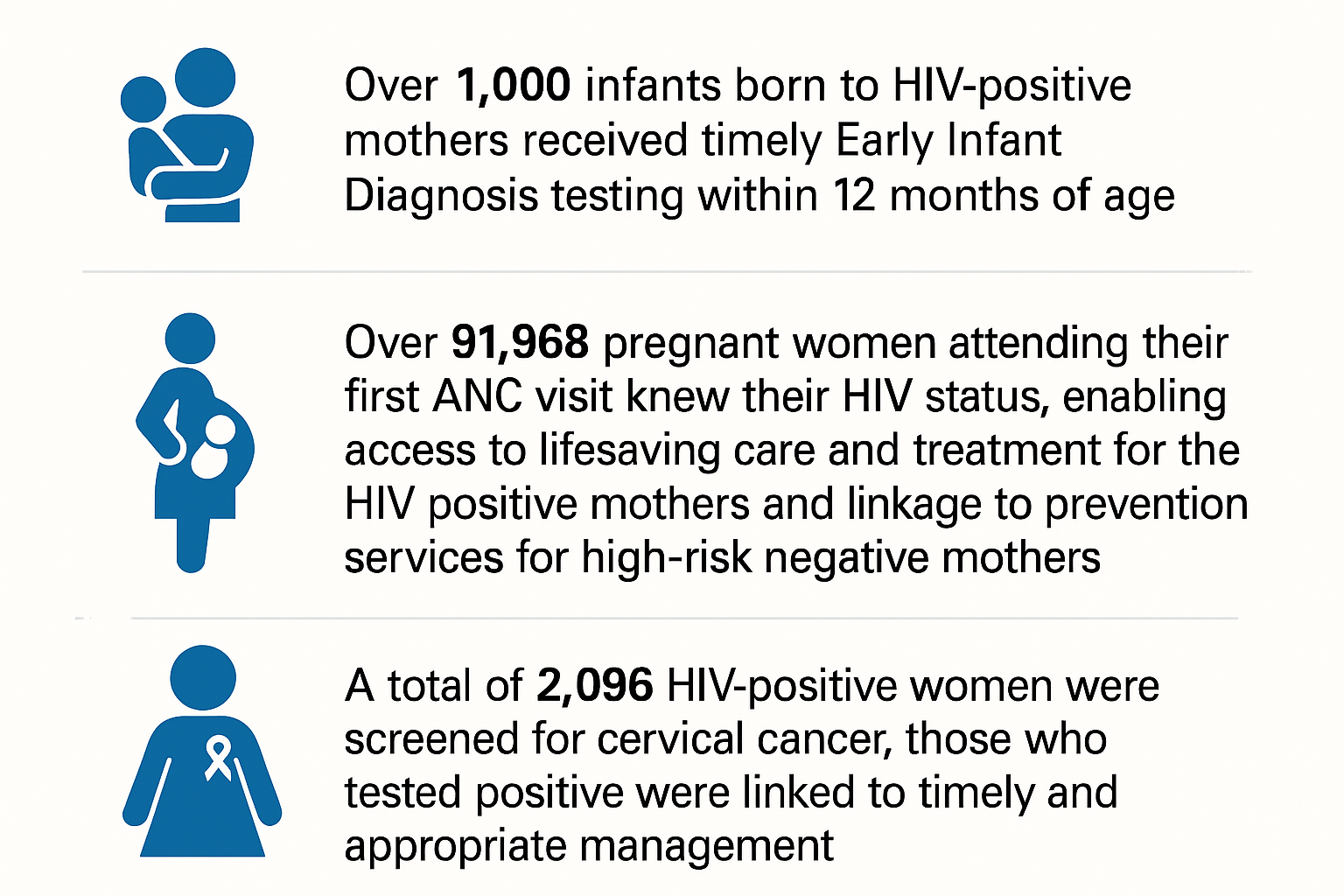
The implementation of the people-centered metrics initiative in the nomadic community demonstrated significant improvements in viral suppression rates among CALHIV. Key outcomes included:
Improved ART Adherence: Through the provision of tailored adherence support and counseling, there was a notable increase in CALHIV adhering to their medication regimen.
Stigma Reduction: Community sensitization programs and support groups led to a reduction in HIV-related stigma, facilitating open discussions and improved mental health among CALHIV.
Enhanced Access to Care: community-based healthcare workers increased the availability and accessibility of healthcare services to CALHIV.
In a period of one year the number of CALHIV patients with non-suppression decreased from 61 CALHIV (in October 2022) to 15 non suppressed clients by September 2023.
Community Empowerment: Engaging the community in the care and support of CALHIV created a nurturing environment that encouraged treatment continuation.
Conclusion:
The people-centered metrics approach proved effective in improving viral suppression among CALHIV in a nomadic community, achieving over 50% increase in viral suppression rates within one year.
Lessons learnt.
Improving viral load suppression for children and adolescents living with HIV requires a holistic approach that considers medical, social, and psychological aspects of care.
Providing age-appropriate counseling and support services is crucial.
Involving parents or caregivers in the care of children and adolescents with HIV is essential.
Implementing adherence support programs, such as reminder systems, peer support groups, can help children and adolescents adhere to their medication regimens consistently.
Collecting accurate and up-to-date data on pediatric HIV cases, treatment outcomes, and program performance is crucial for assessing progress and making informed decisions.